BrIDGs
The Bridging Interventional Development Gaps (BrIDGs) program helps researchers in advancing promising therapeutic agents through late-stage preclinical development toward an Investigational New Drug (IND) application and clinical testing.
Contact
About BrIDGs
The BrIDGs program allows research partnerships to advance candidate therapeutics for both common and rare diseases into clinical testing. Investigators do not receive grant funds through this program. Instead, selected researchers partner with NCATS experts to generate preclinical data and clinical-grade material through government contracts for use in Investigational New Drug (IND) applications to a regulatory branch of authority, such as the U.S. Food and Drug Administration (FDA).
BrIDGs Program Goals
The high cost of translating therapeutic discoveries into clinically available agents can delay the development of promising therapies. Researchers may partner with private-sector companies to advance projects with significant commercial potential, but high-risk ideas or therapies for uncommon disorders frequently do not attract investors.
When private-sector resources are limited, BrIDGs research and development expertise and services can help researchers bridge the gap between the preclinical and clinical stages of therapeutic development. This support allows continued evaluation of agents that may improve the standard of care for patients with a variety of diseases and disorders.
Work With Us
BrIDGs forms partnerships with researchers from academia, nonprofit organizations and pharmaceutical and biotechnology companies to complete preclinical development for promising therapeutic candidates. Contact us to learn more about working with us.
BrIDGs News
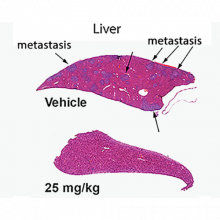
NIH, Northwestern Scientists Develop Potential New Approach to Stop Cancer Metastasis
May 16, 2018 - NCATS News
- Bridging Interventional Development Gaps (BrIDGs)
NCATS scientists collaborated with National Cancer Institute and Northwestern University researchers to identify a new compound, called metarrestin, that blocks the spread of several types of cancer in animal models.
Read ArticleOld Drugs, New Uses: Advances in Drug Repurposing and the Federal Outlook
March 14, 2023 - Media Coverage
- Bridging Interventional Development Gaps (BrIDGs)
- New Therapeutic Uses (NTU)
- Therapeutics for Rare and Neglected Diseases (TRND)
Science Update: Fibroid Risk Associated with Ancestry among Black and White Women, NIH-Funded Study Suggests
July 29, 2021 - Grantee/Partner News
- Bridging Interventional Development Gaps (BrIDGs)
NIH BrIDGs Program Helps Overcome Research Roadblocks
December 4, 2012 - NCATS News
- Bridging Interventional Development Gaps (BrIDGs)
Related Research

Bespoke Gene Therapy Consortium (BGTC)
We help lead this public-private partnership program that focuses on developing platforms and standards to speed the development and delivery of gene therapies for rare diseases.
Platform Vector Gene Therapy (PaVe-GT)
Our pilot project is testing the feasibility of increasing the efficiency of gene therapy clinical trials by using the same gene delivery system and manufacturing methods for multiple gene therapies.

Chemistry Technologies Development
Our chemistry technology experts develop small molecules and screening methods that can be used by other scientists to drive innovations in therapeutic development.


