Building Lung Tissue Models to Speed Virus Drug Testing
February 25, 2021
Although several vaccines are currently available to protect against infection from the virus that causes coronavirus disease 2019 (COVID-19), the development of drug treatments remains a critical medical need and challenge. One reason is the assays, or tests, that are used to find drugs with antiviral activity often are not measuring how a drug behaves in the human body, including its ability to halt the virus from infecting cells and how variant mutations affect this ability and disease severity.
To help solve this challenge, NCATS scientists are developing a cadre of new 3-D tissue models to examine how respiratory viruses like the SARS-CoV-2 virus and influenza viruses can infect the lungs and other tissues and cause disease. They plan to use these models to predict the effects of compounds and drugs against these and related viruses to speed potential treatments to the clinic.
“Our ultimate goal is to have a platform of relevant tissue models on hand to evaluate potential drugs and therapies when the next respiratory virus arrives on the scene,” said Emily Lee, Ph.D., a virologist in the NCATS 3-D Tissue Bioprinting Laboratory (3DTBL).
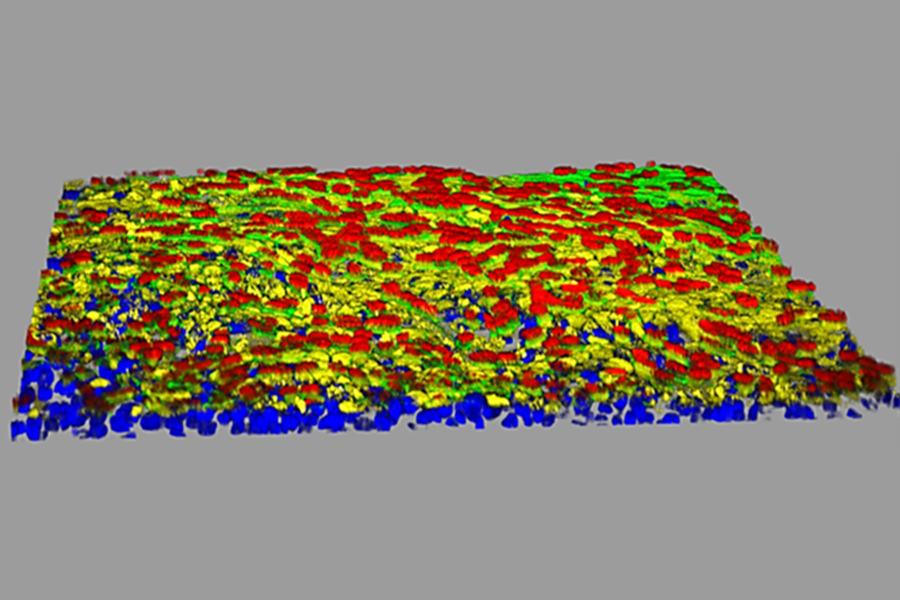
Led by Marc Ferrer, Ph.D., 3DTBL scientists use 3-D tissue engineering techniques to create these laboratory-grown human tissue models that mimic natural tissues in human organs. The tissues live on multiwell plates, where viruses can be added to study how the cells in these tissues are infected and to test the effects of drugs or compounds in halting viral infection. NCATS scientists and others are designing assays to use in experiments, including those in which viruses and their variants can be seen infecting cells as they do in the human body. The experiments will help them determine which drugs and compounds among large collections should be tested in more expensive and time-consuming animal studies.
They also expect that these tissue models will quickly help shed light on whether new mutant variants of the viruses are able to infect cells and whether treatments remain effective.
“3-D tissue models of infected cells can be a bridge to use for rapid, high-throughput screening of thousands of compounds and drugs at once to evaluate potential therapies,” said Lee. “Pandemics are going to keep happening, most likely with respiratory viruses. We want to build a platform where we can plug in any respiratory virus.”
3-D tissue models of infected cells can be a bridge to use for rapid, high-throughput screening of thousands of compounds and drugs at once to evaluate potential therapies. Pandemics are going to keep happening, most likely with respiratory viruses. We want to build a platform where we can plug in any respiratory virus.
Complexity matters
Existing lung tissue models have limited uses in drug testing, Ferrer noted. The NCATS team is using tissue engineering techniques to build different 3-D lung tissue models — some more biologically complex than others — that are made up of various kinds of cells involved in viral infection. The researchers think this strategy will help them study and characterize various aspects of the viral infection process.
For now, the NCATS scientists do not actually work with live SARS-CoV-2 in their laboratories because NCATS lacks the appropriate biosafety laboratory for such experiments. They are, however, studying live SARS-CoV-2 infection in their collaborators’ facilities.
With the help of an intramural award from the National Institute of Allergy and Infectious Diseases’ Intramural Targeted Anti-COVID-19 (ITAC) program, the team is using a technique called single-cell RNA sequencing to determine how and when a viral infection turns which genes on and off in different cell types. They are using these models and single-cell RNA sequencing to study a variety of respiratory viruses in addition to SARS-CoV-2, including various strains of flu and coronaviruses, to better understand the biology of the viral infections in human organs. These studies can provide insights into genetic changes brought on by infections of the different virus variants.
“We’re developing models of greater physiological complexity to see the effects of the virus infection on different cell types, such as those that make blood vessels,” said Ferrer.
His team is creating lung tissues with blood vessels to investigate whether and how SARS-CoV-2 and other viruses play a role in the formation of blood clots, which has been seen in some patients with COVID-19. The team also is working to develop models to examine how the body’s immune system reacts to SARS-CoV-2 infection. In some COVID-19 patients, the immune system unleashes excessive amounts of proteins that trigger inflammation — called a “cytokine storm” — and can lead to acute respiratory distress syndrome, multiple organ failure and other life-threatening complications.
“The benefit of our approach is that we can recapitulate not only the infection, but also the disease aspect,” Lee said. “When we’re testing the effects of drugs on a virus infection in our models, we can screen for broad antiviral effects but also for drugs that can be used against the specific disease.”
These studies may allow the team to observe how a viral infection affects patients with different underlying conditions, such as diabetes or hypertension. As NCATS scientists continue to create innovative, preclinical 3-D cellular models to study the details of viral infections and test promising drugs, one of their goals is to accelerate the development of more individualized therapies as well.