Protein in the Blood Can Help Predict ALS Survival and Decline, Play Role in Developing Treatments
May 13, 2025
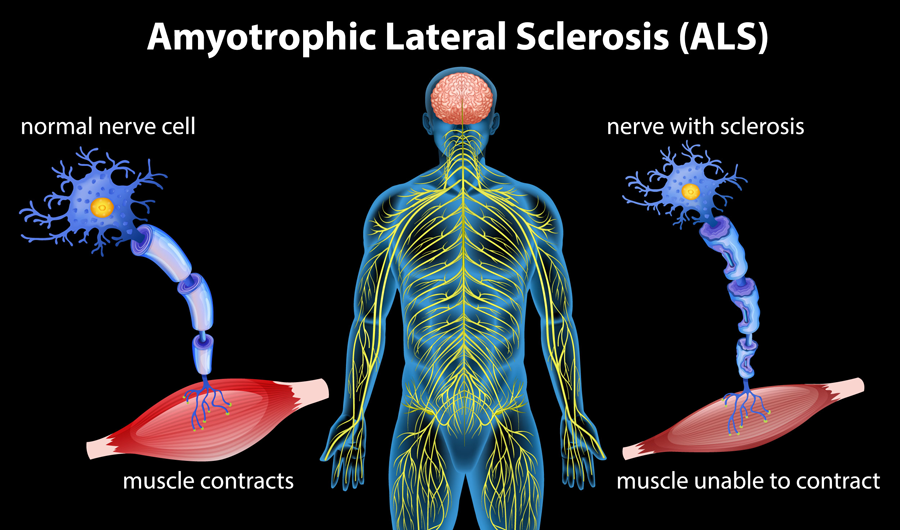
NIH-supported researchers have shown how the level of a protein in the blood — called neurofilament light (NfL) — might be used in developing new drugs to treat amyotrophic lateral sclerosis (ALS). ALS is a rare, progressive disorder that damages the brain and nervous system. ALS has no cure and no effective treatment to slow the disease.
With support from NIH’s Rare Diseases Clinical Research Network (RDCRN), a group of scientists led by Michael Benatar, M.D., Ph.D., at the University of Miami found a link between NfL and ALS. They showed that NfL levels added the most value to clinical predictors of survival time for people with ALS. The results suggest that NfL levels should be considered when designing ALS clinical trials. The researchers reported their findings in eBioMedicine.
ALS affects the brain and spine, causing neurons to die. People lose the ability to move, eventually leading to paralysis and death. But the disease can progress at different rates in different people, complicating the search for effective treatments. The European Network for the Cure of ALS (ENCALS) designed a risk profile model to predict survival time in people living with ALS. The tool consists of a set of clinical predictors and is often used in studies of ALS treatments. Some of those predictors are biomarkers, traits that can be measured in blood or other bodily fluids and soft tissues. Researchers often use biomarkers — in this case, the level of the protein, NfL — to indicate the effects of a treatment or the progress of a disease or condition.
Many biomarkers can be used to track and predict the progression of ALS. But it is unclear which ones add value to the ENCALS score. It is also unclear how each biomarker should be factored into clinical trial design, Benatar explained. Biomarkers come in different “flavors,” depending on their intended use, he noted.
“Prognostic markers measured at the time of initial assessment will tell us something about the future course of disease, like rate of functional decline and survival,” Benatar said. “From a clinical trial design view, we’d like to be able to account for differences among people in how quickly the disease will progress. This will help us design smaller and shorter clinical trials. These markers can help us to discern a therapeutic ‘signal’ within the ‘noise’ of the differences in the disease symptoms among people.”
Benatar and his colleagues wanted to identify the most helpful prognostic biomarkers and explore how they might be used.
The team had already collected data on about 700 people with ALS in a natural history study, charting their disease over time. The researchers looked at blood samples from about 200 people in that study who would have qualified for a clinical trial. That led the team to build a “clinical trial-like” group of patients. The researchers wanted the results to be relevant to the design of future clinical trials.
The scientists found that NfL provides greater prognostic value than the ENCALS predictor score and the combination of NfL and the ENCALS score is a better prognostic measure than either alone. More specifically, the researchers found that pairing the ENCALS score with NfL levels most accurately predicted the rate of functional decline in ALS and the risk of death.
Benatar suggested that initial NfL levels should be considered when analyzing clinical trial data.
“The results of this study are immediately relevant to all ongoing and future ALS trials,” he said. “While there is still much to be learned about NfL, it is clear that its use as a prognostic biomarker should, minimally, be incorporated into the analysis plans of all ALS clinical trials.”
Related Content
Rare Diseases Clinical Research Network (RDCRN)
We oversee this NIH-wide grant program that supports medical research on over 200 rare diseases through clinical studies, including collaborations, study enrollment and data sharing.
Our Impact on Rare Diseases
NCATS is the heart of rare diseases research at NIH. We speed the development of new rare disease treatments by focusing on approaches that can address more than one disease at a time.
A Combination of Tests Shows Learning Capabilities of Nonverbal Children with Rare Brain Disorder
NCATS-funded scientists found that a pair of tests can measure nonverbal learning skills and show the cognitive abilities of children with Aicardi-Goutières syndrome.