Existing Drugs That Safeguard Endoplasmic Reticulum Could Point to Therapies for Many Diseases
June 8, 2021
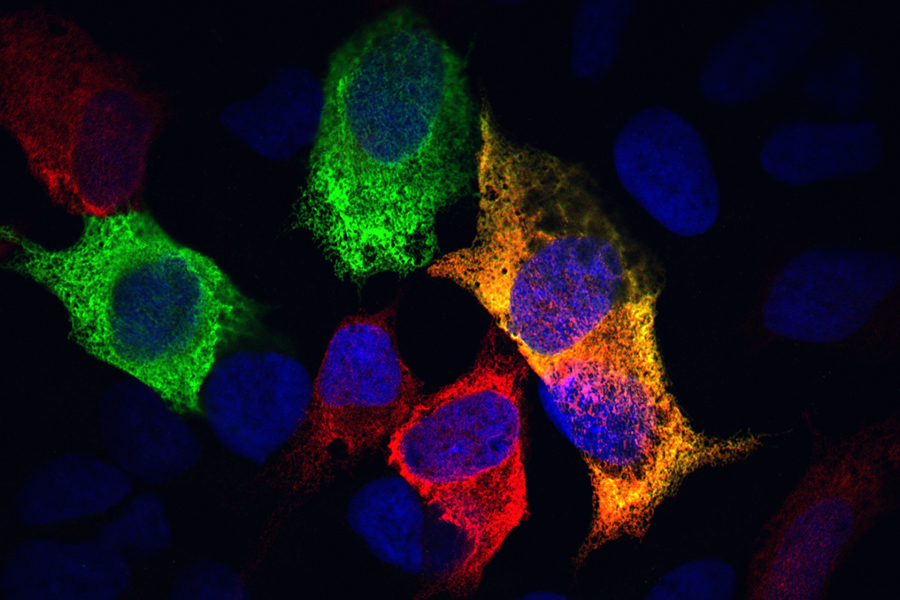
The endoplasmic reticulum, or ER, may not be the first place you’d look to find a culprit in conditions ranging from diabetes and heart failure to Alzheimer’s and chronic hepatitis C. But the ER — a mazelike organelle within every human cell — could offer a powerful therapeutic target in the search for new therapies to curb many conditions.
NIH-funded researchers rapidly screened thousands of compounds within the NCATS Pharmacologically Active Chemical Toolbox and the NCATS Pharmaceutical Collection. They identified five drugs approved by the U.S. Food and Drug Administration (FDA) that keep calcium and proteins in the ER from fleeing — a damaging process that could play a key role in many common and devastating diseases. The researchers’ findings are published in the April 27 issue of Cell Reports.
“The endoplasmic reticulum is central to cellular functions, and ER dysfunction is present in many diseases,” explained NCATS translational scientist Mark Henderson, Ph.D., the study’s co-corresponding author. “The idea behind this research was to look at ER calcium and protein dysfunction and put together a drug screen to find compounds that would restore ER function and foster healthier cells for multiple diseases.”
Just as our bodies have organs that perform key functions, our cells have organelles. The ER is the organelle that serves as the cell’s packaging and shipping center for proteins, as well as a warehouse for calcium storage. To operate effectively, the ER requires high concentrations of calcium. When the ER loses too much calcium, the proteins that perform the organelle’s essential functions escape the ER and exit the cell in a process called exodosis. The loss of ER calcium and the subsequent protein exodosis are linked to neurodegenerative, cardiovascular, musculoskeletal and viral diseases.
To find drugs that maintain healthy calcium levels in the ER and prevent protein exodosis, a research team led by scientists at NCATS and the National Institute on Drug Abuse (NIDA) used quantitative high-throughput screening to test 9,501 compounds at multiple concentrations. That collection of compounds included about 2,500 drugs approved by the FDA.
The researchers used a special technology that tracks ER proteins leaving the cell because of calcium loss to determine how well the screened compounds slowed or stopped ER calcium loss and ER protein exodosis.
They identified 42 FDA-approved drugs that showed anti-exodosis activity and safety for use in cells. The researchers focused on five of the FDA-approved drugs: dextromethorphan, bromocriptine, dantrolene, verapamil and diltiazem.
The research team tested the five drugs’ effects in laboratory cell models of human diseases. Although all of the drugs slowed exodosis in human skeletal muscle cells in which the scientists triggered ER calcium loss, bromocriptine and dextromethorphan had the greatest effect. In a model of Wolfram syndrome, a rare endocrine and neurologic disorder characterized by a genetic change causing ER calcium dysfunction, bromocriptine, verapamil and diltiazem showed effectiveness at maintaining ER calcium. In a cell model mimicking the effects of a stroke, dantrolene and diltiazem cut exodosis and improved cell survival.
Bromocriptine, which is used to treat conditions such as Parkinson’s disease and type 2 diabetes, showed particular promise in models of stroke. A subsequent test in rats demonstrated that bromocriptine and two structurally similar forms of the drug significantly reduced the amount of brain tissue damaged by a stroke, as well as a stroke’s severity. Bromocriptine also showed promise in a mouse model of type 2 diabetes, in which it reduced fasting insulin levels and insulin resistance.
The researchers stated it’s not certain which ER-stabilizing pathways the five tested drugs target, or how the loss of ER calcium and proteins directly affects disease progression. “But if you’re working on a disease where you know that ER calcium is disrupted, and you’re looking for molecules that may have therapeutic efficacy, these compounds are a good starting point,” Henderson noted. “They could offer a fast path to something that could be clinically useful.”
The team is searching for more anti-exodosis compounds. “We have now screened additional libraries beyond those reported in this paper,” explained NIDA scientist Brandon Harvey, Ph.D., the study’s other co-corresponding author. “We have identified molecules with greater potency than any previously found to prevent exodosis.”
The researchers are collaborating with U.S. and international academic research institutes to test anti-exodosis drugs in models of kidney, liver and muscle diseases, as well as models of neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s disease and traumatic brain injury.