NCATS Scientists Turn Stem Cells Into Vast Supply of Neurons to Better Predict Pain Therapies’ Effectiveness
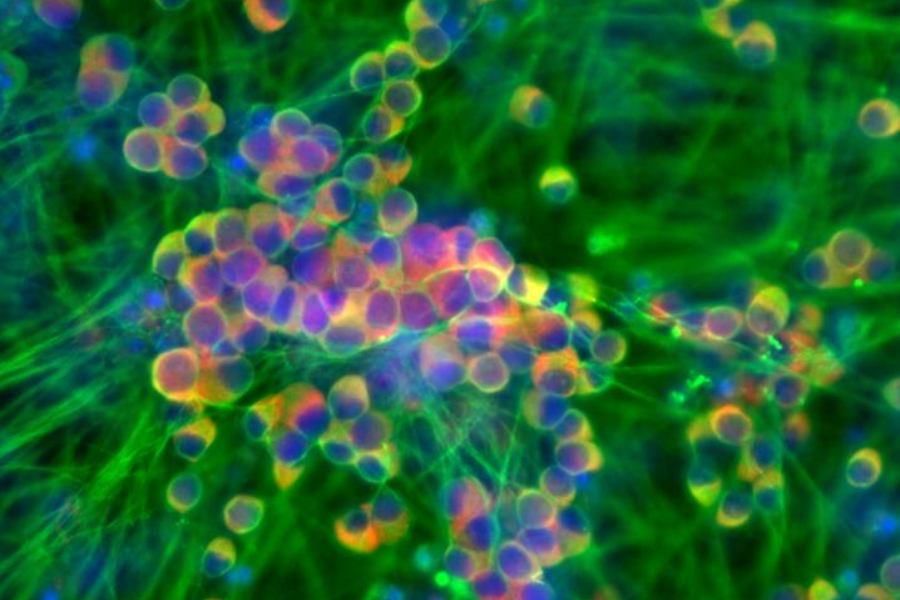
Image shows pain-receptor neurons stained green and red to show cellular activity. (Tao Deng, NCATS Stem Cell Translation Laboratory)
June 14, 2023
An innovative process that quickly turns human stem cells into millions of pain-sensing nerve cells could help researchers speed up the search for new pain therapies. Developed by NCATS scientists, this approach may be a template for other kinds of specialized human cells that are hard to make in large numbers.
Researchers test possible new pain-relieving drugs in the laboratory on nerve cells, or neurons, that sense pain to predict whether a drug might work. But human neurons are available only in limited amounts. Most of the pain-receptor neurons used for testing are from animals or are human cells modified to mimic neurons. But drugs that show promise treating pain in animal neurons or modified human cells fail too often when they are used in people in clinical trials.
“The advantage of our approach is that we’re generating sensory neurons that will better replicate the physiology you would see in a human,” explained Carlos A. Tristan, Ph.D., acting director of NCATS’ Stem Cell Translation Laboratory. The new work appears in the journal Stem Cell Reports.
How Stem Cells Become Sensory Neurons
Human pluripotent stem cells, or hPSCs, can become nearly any type of human cell, such as blood cells, muscle cells or nerve cells. They can also replicate indefinitely. The researchers treated hPSCs with a new NCATS-created mix of small molecules that direct how cells grow. The cell-growth cocktail steered the stem cells down a development path to become pain-receptor neurons. The scientists then used a method that NCATS invented to protect and preserve the sensitive cells.
The nerve cells made from hPSCs had the functional and cellular features of human pain-receptor neurons. They also had many of the genes, molecular markers and possible targets for treatments that are important for pain research.
The new approach proved to be reproducible. The NCATS team’s colleagues at Boston Children’s Hospital, Harvard Medical School and Sophion Bioscience followed the stem cell protocol and made their own fully functional human pain-receptor neurons.
“In the stem cell field, reproducibility is a major roadblock,” explained Vukasin Jovanovic, Ph.D., the study’s co-lead author and a postdoctoral fellow in NCATS’ Stem Cell Translation Laboratory. “We tried to develop a protocol that is highly reproducible and efficient.”
NCATS researchers also worked to make the process fast and effective on a large scale. The team automated the development journey by using a robotic cell culture system, which allowed the scientists to make the new cells rapidly and in large amounts. They grew more than 150 million nerve cells in 14 days — and the robotic cell culture system could deliver 30 times that number. At that volume, pain researchers could use high-throughput screening to test many possible treatments quickly.
“Using our novel approach, we can now rapidly and reproducibly generate large amounts of sensory neurons,” Jovanovic said. “That will pave the way for accelerated testing of potential pain therapies and more accurate predictions of their effectiveness and safety in humans.”
The protocol will see action soon with pain researchers working on the NIH Helping to End Addiction Long-term® Initiative, or NIH HEAL Initiative®. Research related to the initiative will use the hPSC-derived pain-receptor neurons to explore gene editing approaches to control pain, model chemotherapy-induced peripheral neuropathy and understand the mechanisms that drive diabetic peripheral neuropathy.


