Collaboration to Enhance Naloxone Distribution in Rural Areas
Opioid misuse in the United States has reached pandemic proportions and represents a significant public health problem, with rural areas being disproportionately affected. To address this health crisis, a range of strategies are being implemented, including the use of naloxone, an opioid antagonist medication. Pharmacists are the most accessible health care providers in rural and medically underserved areas, and recent legislative efforts in many states have increased access to naloxone through statewide standing orders and pharmacist prescriptive authority. Nevertheless, multiple barriers still hinder effective pharmacy-based naloxone distribution.
To address this translational gap, The University of New Mexico Clinical and Translational Science Center (CTSC) (Principal Investigator: Richard Larson, M.D., Ph.D.; Project Co-Directors: Ludmila Bakhireva, M.D., Ph.D., M.P.H., and Theresa Cruz, Ph.D.) led a collaborative Project CONsiDER with Clinical and Translational Science Award (CTSA) Program hubs at Tufts University (Thomas Stopka, Ph.D., M.H.S.) and the University of Minnesota (Laura Palombi, Pharm.D., M.P.H., M.A.T., AE-C) to develop an innovative and sustainable model to increase the dispensing of naloxone by community pharmacists practicing in rural and underserved areas. The UNM CTSC became interested in leading this research because New Mexico has one of the highest rates of opioid overdose in the country. Additionally, New Mexico is a largely rural state, ranking fifth in size among the 50 states, with a total population of 2.1 million. New Mexico is also ethnically diverse, with a population that is 49.1% Hispanic and 10.9% American Indian. The UNM CTSC partnered with the University of Minnesota and Tufts University Clinical and Translational Science Institutes because of their aligned interests in addressing the opioid epidemic in rural areas.
The study focused on dissemination and implementation science, which addresses a T3 “translational gap” between scientific discovery and routine practice. The goal was to improve public health by improving the health care delivery system in rural communities. Specifically, we aimed to increase naloxone dispensing by pharmacists by adapting an evidence-based intervention to the local context in New Mexico, Minnesota and Massachusetts, and then implementing the intervention, which focused on pharmacist training regarding naloxone and naloxone dispensing. We first engaged community stakeholders in each state, including community pharmacists, the state Departments of Health, the state Boards of Pharmacy and professional organizations. These partners collaborated with us to identify core elements of the pharmacy education materials, as well as state-specific modifications (e.g., information about state pharmacy laws regarding naloxone dispensing) to bolster local relevance to pharmacy staff and customers. Their input informed the adaptation and implementation of the intervention in different contexts. We then pilot tested the intervention at community pharmacies in each state. The training focused on pharmacological information regarding naloxone, communication skills, strategies for reducing stigma and guidance regarding how to operationalize naloxone dispensing. The trainings were conducted in person, at the pharmacy, with a follow-up visit to address site-specific implementation challenges. It captured both pharmacists and pharmacy technicians and included staff- and patient-oriented materials. Baseline and follow-up surveys were conducted with participating staff to assess changes in naloxone distribution, as well as changes in attitudes, self-efficacy and intent with regard to naloxone distribution.
Several challenges were encountered during the study, including staff turnover, need to secure management support for participation, travel distances for the research teams, variable work schedules for participants and time for participation. The research team employed several strategies to mitigate these challenges. A pharmacist on the research team sought regional approval from pharmacy chain managers for the program. Additionally, the team engaged pharmacy students to help with pharmacy operations at training sites under the guidance of a College of Pharmacy preceptor. This allowed the pharmacy to continue functioning while pharmacists and technicians participated in the training. The team also needed to be flexible regarding when to conduct the trainings to fit into pharmacy schedules. Lastly, although travel distances to rural areas remain a barrier to intervention implementation, several strategies are recommended to mitigate the challenge. These include training pharmacist trainers in different regions of the state, developing online materials to supplement the in-person training and training multiple pharmacies in a region on the same trip.
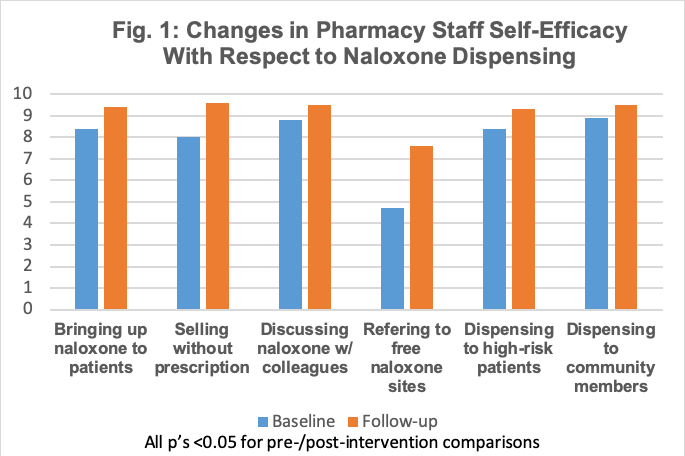
Although there was some variability by state, overall accomplishments of the project included establishing the feasibility of implementation in rural communities, increasing knowledge and self-efficacy regarding naloxone and naloxone dispensing, and minimizing stigma associated with opioid overdose prevention (Figure 1). Preliminary results also indicate substantial increase in naloxone dispensing post-intervention in participating sites. Pharmacists participating in the study also reported on the benefits of the intervention. One participant, addressing the communication skills component of the training, stated, “I think the training made me rethink how to address naloxone with patients.” Another pharmacist commented, “I really enjoyed the role play. It helped me apply information in a realistic way.” Pharmacists also noted the importance of including technicians in the trainings, because technicians play a leading role in interactions with pharmacy customers.
Because of the successful outcomes of the pilot study, the New Mexico Department of Health is supporting the New Mexico research team in the dissemination and evaluation of the intervention throughout the state. This model demonstrates a successful testing of a novel intervention via the CTSA network followed by a statewide dissemination supported by local agencies.
This multistate collaborative approach among three CTSA Program hubs directly addressed NCATS’ goal of “a more integrated and collaborative national network.” By leveraging the resources of the CTSA Consortium, the CONsiDER Project developed a robust implementation model tested in differing contexts (e.g., differing naloxone policies, unique opioids, differential access to care, and varied population demographics) that is scalable throughout the country through the CTSA consortium.
For questions about the CONsiDER Project and training materials, please contact Dr. Ludmila Bakhireva or Dr. Theresa Cruz.