Addressing Health Disparities and Improving Rural Health
The Institute of Translational Health Sciences is strongly committed to addressing health disparities and improving rural health across the Washington, Wyoming, Alaska, Montana and Idaho (WWAMI) region.
The University of Washington Institute of Translational Health Sciences is strongly committed to addressing health disparities and improving rural health across the Washington, Wyoming, Alaska, Montana and Idaho (WWAMI) region. A key mechanism for this work is the effort of the WWAMI region Practice and Research Network (WPRN), which supports collaboration between primary care practices and academic researchers on research that improves the health and well-being of patients in their communities and enhances primary care clinical practice.
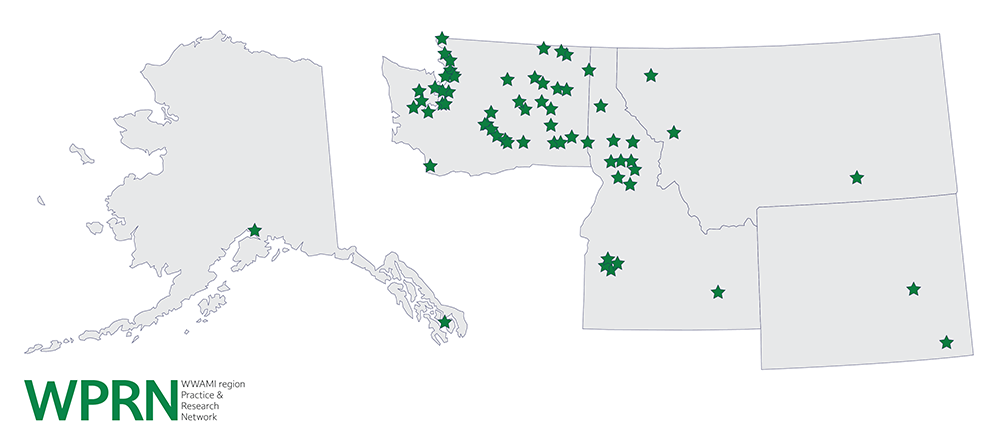
The WPRN is a practice-based research network of more than 120 primary care practices in the five-state WWAMI region. These clinics include community health centers, private and academically affiliated practices, and government-operated clinics. These clinics are spread throughout the WWAMI region, which covers 27% of the land mass of the United States and includes vast rural areas with both minority and underserved populations [Figure 1].
The University of Washington’s School of Medicine serves the WWAMI region, with more than 95% of acceptances coming from applicants in the region. The WPRN was formed in this environment in partnership with the WWAMI region educational programs in the Department of Family Medicine, specifically the Family Medicine Residency Network (FMRN). Programs in the FMRN were interested in increasing their research activities, and the WPRN provided an opportunity for regional practices and residency sites to participate and collaborate in translational research.
Because medical needs in rural areas are largely met by primary care, improving the health of rural communities requires engaging the primary care practices that serve them. With this goal in mind, the WPRN developed a research model that includes site clinical research champions supported by a coordinating center that facilitates participation by small rural practices. The WPRN has focused on geographic diversity to ensure that rural health needs are recognized and that rural populations can participate in cutting-edge research. The WPRN coordinating center has recruited diverse champions and focused on engagement strategies that can succeed in resource-limited rural settings. Multiple opportunities for inclusion are incorporated, ranging from annual meetings, a survey research panel, and engagement projects that focus on issues driven by the community.
With this infrastructure and these relationships, within the past 15 years, the WPRN has been able to support more than 80 projects, 60 publications and 200 grant applications related to rural health. One of the most visible successes from this work is the development of Data QUEST, a shared electronic health record network containing data from more than 220,000 patients. These patients span more than 3,000 providers and 25 clinics, 60% of which are rural or rural-serving and support observational studies and pragmatic clinical trials.
Another major accomplishment is Team-Based Safe Opioid Prescribing, a project that created the Six Building Blocks Program team-based approach for more selective and cautious opioid prescribing for chronic non-cancer pain across 20 rural health clinics. The Six Building Blocks Program provides a roadmap for redesigning and improving a clinic’s management of patients who are on long-term opioid therapy for chronic pain. This program began as an observational study of best practices that then developed into an intervention rigorously tested in rural practices that has been widely disseminated. The number of patients using long-term opioid therapy decreased by 14% over 15 months in the Six Building Blocks clinics—from 2,065 to 1,776. Additionally, the proportion of patients on high-dose opioids (≥ 100 MED daily) decreased 20% within the program, from 11.8% to 9.6%. Clinicians and staff across the rural-serving clinics enrolled in Six Building Blocks reported that the program improved their work-life experience and their ability to provide high-quality care. They reported increased confidence and comfort in providing care, enhanced collaboration and teamwork, and improved relationships with patients. The Six Building Blocks program is now being disseminated regionally and nationally, with dozens of practices impacting thousands of patients through grants and contracts with the National Institute on Drug Abuse, the Washington State Department of Health, the Agency for Healthcare Research and Quality and the Olympic Community of Health. A Six Building Blocks implementation toolkit has also been developed.
In achieving its success, the WPRN has overcome multiple barriers, none so difficult as the wide distances between primary care practices. To prevent geographic limitations from causing issues with clinic integration and engagement, the WPRN uses telework strategies to foster and maintain a high level of engagement across the network. The WPRN also hosts an annual full-day conference in Seattle to bring site champions together face-to-face, conducts webinars to onboard new studies across the network, and—most importantly—ensures that all research results are returned to the clinics for studies on which they have collaborated. Another common barrier to inclusion of remote care facilities in research is combating the expectations of urban researchers. Frequently, resource-rich research institutions assume incorrectly that rural centers will be unable to carry out research for budgetary or feasibility reasons. Strategies implemented through the WPRN, including novel remote recruitment plans and virtual focus groups, have shown that this presumption need not be the case.
Misconceptions about the capacity and quality of rural research centers are a significant roadblock for many institutions that attempt to conduct research on rural health and heath disparities. The WPRN has shown over the years that rural communities and practices are accomplished and should not simply be considered smaller versions of urban communities and practices. Rural settings have their own ecosystems and contexts that are critical to understand and consider when conducting collaborative research. Strong relationships and bidirectional partnerships make this work possible. It cannot be stressed enough that translational research should not be unidirectional; the academic institution does not always bring discovery to rural communities. There is an enormous amount of innovation in rural communities, and Clinical and Translational Science Award (CTSA) Program hubs have the opportunity and the obligation to identify those health innovations, empower researchers in the field, and provide tools and resources so that each CTSA Program institution can perform research with rural communities, rather than on rural communities.
To learn more about the Institute of Translational Health Sciences, please visit www.iths.org.
For more information about the WWAMI region Practice and Research Network, please visit www.iths.org/community/partners/crn/wprn/.
For more information on the Six Building Blocks Program, please visit www.ahrq.gov/patient-safety/settings/ambulatory/improve/six-building-blocks.html.