NIH Funding Bolsters Rare Diseases Research Collaborations
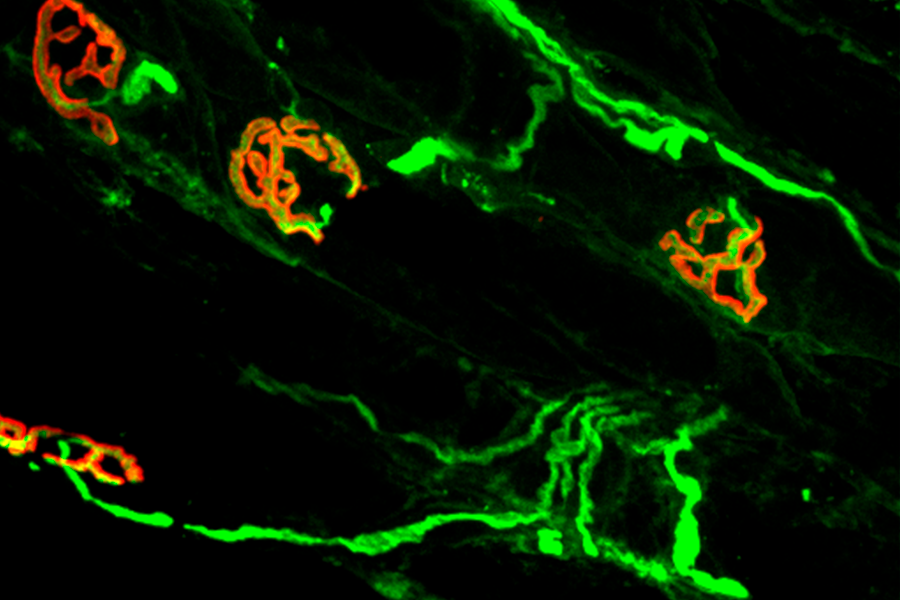
Researchers from the RDCRN-supported Myasthenia Gravis Rare Disease Network are studying rare, chronic autoimmune diseases that affect how well nerves and muscles communicate with each other. Neuromuscular junctions, where motor nerves (green) send signals to muscles (red), are shown here. (Xiangyang Zhang, Ph.D., The George Washington University School of Medicine & Health Sciences)
October 3, 2019
New grants aimed at better understanding diseases, moving potential treatments closer to the clinic
Of an estimated 6,500 to 7,000 known rare diseases, only a fraction—maybe 5%—have U.S. Food and Drug Administration-approved treatments. To increase that percentage, the National Institutes of Health has awarded approximately $31 million in grants in fiscal year 2019 to 20 teams—including five new groups—of scientists, clinicians, patients, families and patient advocates to study a wide range of rare diseases. An additional $7 million has been awarded to a separate data coordinating center to support these research efforts.
The grants, which support consortia that together form the Rare Diseases Clinical Research Network (RDCRN), are aimed at fostering collaborative research among scientists to better understand how rare diseases progress and to develop improved approaches for diagnosis and treatment. This is the fourth five-year funding cycle for the RDCRN, which is supported by multiple NIH Institutes and Centers and led by NIH’s National Center for Advancing Translational Sciences (NCATS) and the NCATS Office of Rare Diseases Research.
Individually, most rare diseases affect only a few hundred to several thousand people; collectively, rare diseases affect more than 25 million Americans. Many rare diseases are life-threatening and about half of those affected are children.
Because rare diseases affect a small number of people, they can be extremely challenging to study. Scientists often lack basic information about a rare disease’s symptoms and biology, and the ways a disease can affect people over time. Research funding can be scarce.
“Over the years, RDCRN scientists have partnered with patients and advocates to develop new insights into the causes and progression of—and potential therapies for—rare diseases that were simply not receiving the attention they deserved,” said NCATS Director Christopher Austin, M.D. “Their pioneering work in discerning underlying clinical differences and commonalities in hundreds of rare conditions has already changed the rare disease landscape in immeasurable ways.”
Established by Congress under the Rare Diseases Act in 2002, the RDCRN has included more than 350 sites in the United States and more than 50 in 22 other countries. To date, they have encompassed 237 research protocols and included more than 56,000 participants in studies ranging from immune system disorders and rare cancers to heart and lung disorders, brain development diseases and more.
Each RDCRN member is a consortium of clinical and scientific experts and patient groups who study a group of rare diseases. Each consortium must study three or more diseases, partner with rare disease patient advocacy groups, provide rare disease research training to investigators and perform natural history studies that chart the course and progression of diseases. The primary focus of the RDCRN is clinical research, and the network does not generally support clinical care outside of research activities.
A key component of the RDCRN is the Data Management and Coordinating Center (DMCC), which was awarded to the Cincinnati Children’s Hospital Medical Center. The DMCC manages shared resources and data from the RDCRN research studies. The DMCC emphasizes the standardization of data, increased data sharing and broad dissemination of research findings.
The RDCRN consortia have a rich history of accomplishment. For example, Lysosomal Disease Network scientists led crucial natural history studies and gene editing research that provided a foundation for first-in-human genome editing clinical studies for a rare metabolic disease. Primary Immune Deficiency Treatment Consortium members showed the advantage of early stem cell transplants for patients with a rare immune system disorder, severe combined immunodeficiency, and the group’s work contributed to advances in gene therapy-based treatments for the disease.
New groups, new emphasis
The five new consortia are:
- The Global Leukodystrophy Initiative Clinical Trials Network. Lead: Children’s Hospital of Philadelphia
- Congenital and Perinatal Infections Rare Diseases Clinical Research Consortium. Lead: The University of Alabama at Birmingham
- Frontiers in Congenital Disorders of Glycosylation. Lead: Mayo Clinic, Rochester, Minnesota
- Hyperphenylalaninemia Disorders Consortium. Lead: Oregon Health & Science University, Portland
- Myasthenia Gravis Rare Disease Network. Lead: The George Washington University, Washington, D.C.
According to ORDR director Anne Pariser, M.D., an important focus of the latest group of awards is on clinical trial readiness.
“Some of the RDCRN research groups have been working together for 10 or 15 years and have gathered important data and developed a good understanding of the diseases they study, in addition to new potential therapies. We’re emphasizing the need to be prepared to conduct clinical trials,” Pariser said.
“We’re trying to get the drug candidates closer to be ready for clinical testing and de-risk the processes that lead to a successful clinical trial,” said RDCRN program officer Tiina Urv, Ph.D. “To get funding to conduct trials, they need to have strong natural history studies that show how the disease progresses, ways to measure outcomes of treatments and biomarker studies that provide indicators of how a drug is working in patients.”
Collaboration is key. Consortia can involve numerous partner research teams from different sites, along with rare disease patients and advocacy groups. Scientists from different institutions come together to pool patients, data, experience and resources.
“Scientists can’t work alone. They wouldn’t have enough patients, and they wouldn’t have adequate resources and information about the diseases,” Urv said. “Patients and families help scientists decide what is important to study, test and treat.”
To read more about the five new consortia, 15 continuing consortia and the DMCC, see: https://ncats.nih.gov//research/research-activities/rdcrn/consortia.
In addition to NCATS, other NIH funding support comes from the National Institute of Allergy and Infectious Diseases, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute of Neurological Disorders and Stroke, the National Heart, Lung, and Blood Institute, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Dental and Craniofacial Research, the National Institute of Mental Health and the Office of Dietary Supplements.
About the National Center for Advancing Translational Sciences (NCATS): NCATS conducts and supports research on the science and operation of translation—the process by which interventions to improve health are developed and implemented—to allow more treatments to get to more patients more quickly. For more information about how NCATS is improving health through smarter science, visit https://ncats.nih.gov.
About the National Institutes of Health (NIH): NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit https://www.nih.gov.


