Meet Chip: Disease Models
Patients suffering from disease need treatments that are more effective and have fewer side effects. Consequently, scientists need faster, more efficient ways to test experimental drugs and help gain approvals for use in the clinic. New technologies that show promise toward meeting these goals include 3-D disease models, such as chip devices with human tissue, that simulate human physiology — approaches that may help better predict how the drugs will actually work in humans.
NIH-supported teams of scientists are working on several tissue chip models that recapitulate key aspects of human disease, with the aim of learning more about these devastating conditions and designing new treatments.
Metastatic Breast Cancer in the Liver
Up to 30 percent of women with early-stage breast cancer will relapse eventually when the cancer spreads to the liver or other parts of the body through a process called metastasis. Metastatic breast cancer in the liver cannot be cured, but the disease can be controlled, sometimes for many years.
NIH-supported scientists at the Massachusetts Institute of Technology and University of Pittsburgh have developed a 3-D system that keeps human liver tissue alive and functioning for a month or more in the laboratory. The chip mimics conditions in the human body, something that is impossible in animals or other model systems. This LiverChip system is then “seeded” with breast cancer cells, creating a model of metastatic breast cancer in the liver.
The team is using this bioengineered system to learn more about:
- How breast cancer cells multiply in the liver
- How the cancer cells interact with the normal liver cells in a way that protects the cancerous cells from the body’s defenses
- How the cancer cells respond to chemotherapy
Rare Heart and Muscle Condition
Barth syndrome is a rare genetic condition that occurs almost exclusively in men. The disease weakens the muscles, including the heart, which becomes dangerously enlarged. Barth syndrome can lead to heart failure, a life-threatening condition in which the heart cannot pump enough blood to meet the body’s needs.
Barth syndrome is caused by a mutation in a gene called TAZ that affects how mitochondria work in muscle cells. Mitochondria function as cell “power stations” by generating energy for the rest of the cell to use. The damaged TAZ gene in muscle cells stops normal production of TAZ protein, which leads to a poorly functioning heart.
To better understand Barth syndrome, NIH-supported researchers at Harvard University developed a way to grow heart muscle cells on a chip. The researchers generated cardiac cells from induced pluripotent stem cells (iPSCs) derived from adult donor cells. Stem cells have the remarkable potential to develop into many different cell types. Stem cells are important during early life and for embryonic growth; in adults, stem cells function in tissue repair and maintenance. iPSCs can produce an unlimited supply of donor cells capable of forming heart and other types of tissues for the chip devices. The cells on the cardiac chip can even beat synchronously like a real human heart.
When the researchers used iPSCs from a person with Barth syndrome to construct cardiac chips, the heart tissue displayed a weakened heartbeat and poorly organized structure, creating a model that mimics a Barth syndrome patient’s heart.
When the researchers introduced a normal form of TAZ protein back into the heart cells on the Barth syndrome chip, the cells began beating strongly again. The team observed the same beneficial effect in the presence of a synthetic compound, suggesting the heart chip may soon be used to test drugs for this currently incurable disease. Promising new leads could be tested on the Barth syndrome chip to determine whether the heart cells function as expected before testing the drugs in patients.
Tumor with Blood Vessels
Cancer drugs are supposed to be toxic; that’s how they kill tumor cells. However, they also can kill healthy cells in other areas of the body. For example, the drug trastuzumab (Herceptin), which is used to treat some types of breast and stomach cancer, can cause congestive heart failure and other heart problems.
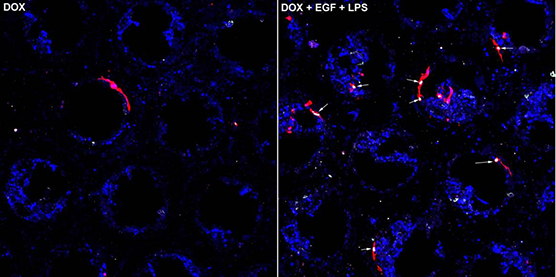
Researchers at Washington University in St. Louis and the University of California, Irvine, are developing a chip to study tumors in their natural environment, supported by tiny blood vessels. Studies have shown that tumor cells behave differently when grown in three dimensions as opposed to the more traditional approach of a single, flat layer. In a 3-D system, tumor cells have different shapes and are more resistant to cancer drugs. Testing drug candidates on a 3-D chip gives researchers a more realistic idea of the drug’s chances against a tumor growing in a human body.
The tumor chip includes functioning blood vessels, which tumors in the body need to stay alive. Some cancer drugs target the blood vessels that supply tumors in the hope of starving the tumor cells. However, these drugs may also affect blood vessels in other areas of the body, with the potential to cause high blood pressure and blood clots. The tumor chip may help researchers find a balance between attacking tumors and protecting blood vessels.
The tumor chip also could be linked to heart and bone marrow tissue, both of which can be damaged by cancer drugs. This approach would enable the researchers to study how drug candidates affect these tissues as well.
Looking Ahead
Once these models are integrated with chips based on other human organs, scientists will be able to learn more about how other body systems affect diseases. For example, scientists could study how the immune system affects the activity and growth of metastatic tumors or how experimental treatments for heart failure affect other organs.
Ultimately, scientists might use this technology for precision medicine to predict which treatments would be most effective against a person’s specific disease while minimizing side effects. Scientists might use the LiverChip to identify optimal conditions for administering chemotherapy drugs, for example, during morning or evening, in a fasting state or on a full stomach.
In September 2017, NCATS and its NIH collaborators announced 13 awards for the Tissue Chips for Disease Modeling and Efficacy Testing initiative.