2018 Tissue Chips for Modeling Diabetes
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and NCATS support the development and validation of human tissue chips that closely mimic the normal physiology of key metabolic tissues, including the pancreatic islet, liver, skeletal muscle and white adipose tissue. Ultimately, the goal is to combine the human metabolically active tissue chips with immune system components to develop a fully integrated model of immune-mediated metabolic dysfunction, as a first step toward the generation of in vitro models for human type 2 diabetes and other metabolic diseases.
These projects are funded by NIDDK with additional support from NCATS:
Cincinnati Children’s Hospital Medical Center
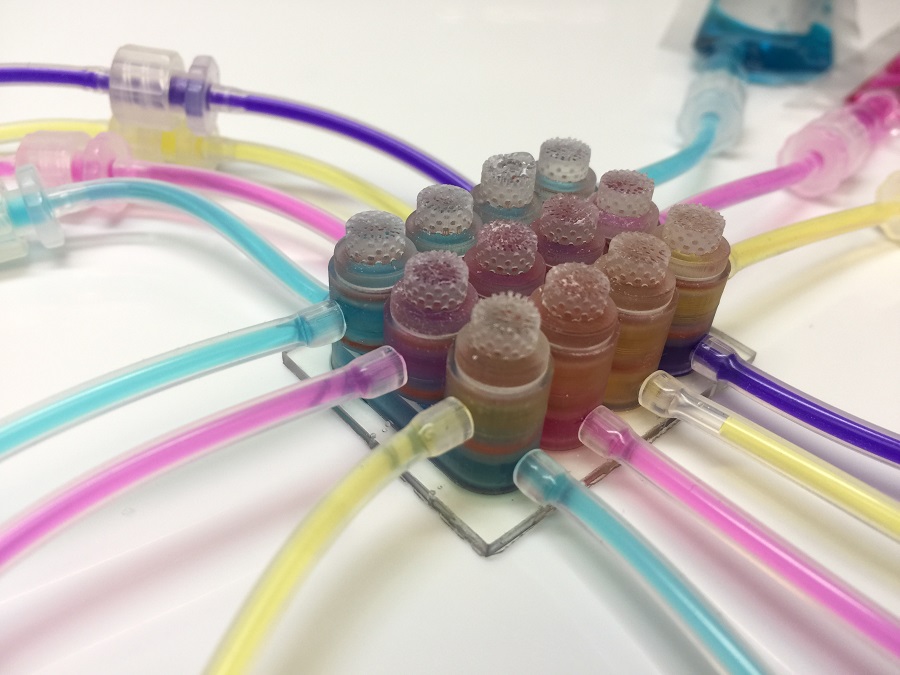
Modeling Diabetes Using an Integrated Plate System
Principal Investigators: James M. Wells, Ph.D., and Moo-Yeal Lee, Ph.D.
Grant Number: 1-UG3-DK119982-01
University of California Berkeley
Microphysiological Systems to Interrogate the Islet-Liver-Adipose Axis in Normal Physiology and Type 2 Diabetes Mellitus
Principal Investigators: Andreas Stahl, Ph.D., Kevin Edward Healy, Ph.D., Matthias Hebrok, Ph.D., Edward C. Hsiao, M.D., Ph.D., and Holger Willenbring, M.D., Ph.D.
Grant Number: 1-UG3-DK120004-01
University of Pittsburgh at Pittsburgh
Human Microphysiology Systems Disease Model of Type 2 Diabetes Starting with Liver and Pancreatic Cells
Principal Investigator: Taylor D. Lansing, Ph.D.
Grant Number: 1-UG3-DK119973-01