Meet Chip: Heart
The heart is the center of the circulatory system, which consists of a network of blood vessels: arteries, veins and capillaries. The heart uses electrical signals to contract the muscular walls and pump blood into the circulatory system.
A healthy heart supplies the body with the right amount of blood at the rate needed to work well. If disease or injury weakens the heart, the body’s organs won’t receive enough blood to work normally. Drugs also can change the rate and regularity of a heartbeat. Consequently, scientists need to be able to better predict which drugs might have toxic effects.
Current testing, which is done in animal models and laboratory tests, is not always accurate enough to predict toxicity in humans. In fact, toxic effects on the heart are among the most common reasons that a new drug fails in the human testing phase or even after the drug is on market, and this cardiotoxicity accounts for one-third of market withdrawals.
Heart on a Chip
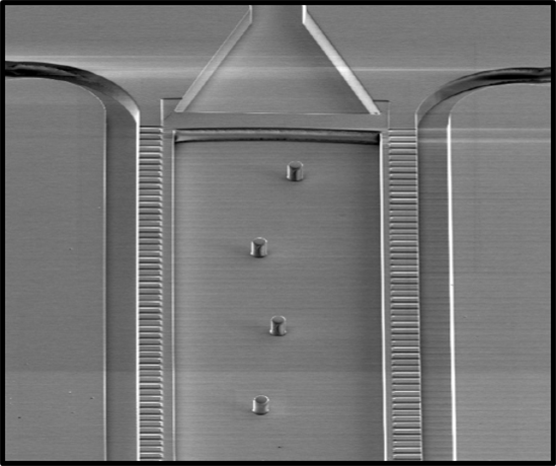
A team of researchers(link is external) at the University of California, Berkeley, have integrated cardiac cells in a heart on a chip. The researchers generated cardiac cells from induced pluripotent stem cells (iPSCs) derived from adult donor cells. Stem cells have the remarkable potential to develop into many different cell types. Stem cells are important during early life and for embryonic growth; in adults, stem cells function in tissue repair and maintenance. iPSCs can produce an unlimited supply of donor cells capable of forming heart and other types of tissues for the chip devices.
The chip provides nutrients and oxygen to keep the cells alive. The resulting heart tissue even has a heartbeat. When the researchers used iPSCs from a patient with a disease that causes a slow heart rate, the “pulse” of the cardiac chip was slower than in chips bioengineered from iPSCs from a healthy adult, showing that cardiac tissue keeps some key characteristics, even when grown in plastic.
In this video, the left panel shows the chip with heart tissue beating at a normal rate. When a drug called isoproterenol is added (right panel), the heart rate becomes faster, mimicking the response in human patients.
Heart, Microvessels and Liver on a Chip
NIH-supported research teams from Columbia University, the Massachusetts Institute of Technology, Boston University, the Wyss Institute at Harvard University and Yale University are growing cardiac cells from iPSC lines and allowing them to mature on a heart chip that will mimic heart cell function in the body.
The scientists on this project are assembling an integrated human circulation-liver-heart model system that mimics the coordinated function of the human body. By using iPSCs from healthy individuals and patients carrying various diseases, the teams are personalizing the system to model specific genetic and disease states and test therapeutics for effectiveness and toxicity in the heart and other organs.
Looking Ahead
The teams of scientists envision using the heart on a chip in conjunction with other organ-on-chip devices to screen candidate drugs for toxic side effects. The ability to screen potential drugs accurately in such models could be an advance over the use of animal models, which can be relatively expensive and, of more concern, fail to predict dangerous reactions. These systems also will enable scientists to model rare genetic disorders to investigate treatment options.
When the tissue chips are linked together, almost like a “human on a chip,” researchers may be able to predict a drug’s effects on many organ systems simultaneously.