Meet Chip: Blood Vessels
Scientists are interested in finding new technologies to study blood vessels for several reasons:
- Heart disease and clogged arteries are a major cause of disability and death due to heart attacks and strokes. Drugs to treat heart disease and high blood pressure act on the cells of blood vessels.
- Blood vessels transport drugs throughout the body, bringing the drugs to organs or tissues where they are needed.
- Drugs used to treat childhood cancers can damage the cells lining blood vessels, increasing the risk for cardiovascular disease.
- Many cancerous tumors secrete growth factors to stimulate the development of blood vessels. This process diverts nutrients and oxygen away from healthy tissues to support the abnormal, rapid growth of the cancer. In addition, the cancer can metastasize (spread) to other areas of the body through blood vessels. Patients could benefit from treatments that stop the growth of these blood vessels.
NIH-supported scientists are developing a series of human tissues and organs on chips for testing the safety and effectiveness of potential new treatments, and these systems also can help researchers study diseases. Several of these organs on chips include blood vessels to ensure that the living tissues continue to function and allow drugs to travel as they would in the human body.
Blood Vessels on a Chip
Through bioengineering — the science of creating complex, functional tissue from cells — Duke University scientists have generated human blood vessels on a chip. Not only can the bioengineered vessels deliver oxygen and nutrients into the tissue, but they also can contract and dilate just like blood vessels in the human body do to help regulate body temperature and metabolism.
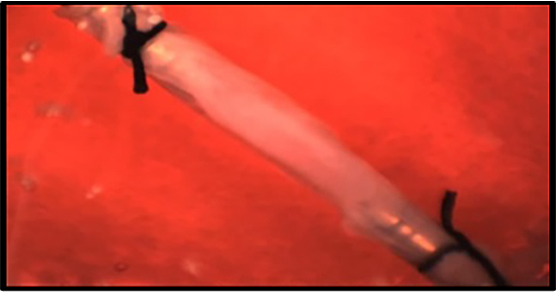
The video shows white blood cells (fluorescing red) passing through the vessel. The white blood cells (red) can attach to the blood vessel wall (blue) and travel into the tissue to fight infection, similar to what occurs in the body.
Functional microvessels derived from induced pluripotent stem cells form networks capable of fluid flow. In this video, fluorescent purple beads show functional flow in the vessels. Colon cancer cells (green) can grow nearby, mimicking the human cancer microenvironment.
This video shows green fluorescent beads flowing through the microvessel.
Looking Ahead
The teams of researchers working on blood vessels and microvasculature envision using the technologies to link other tissue chip devices. The result would be a continuous network linking multiple organs. With such a system, scientists could learn about new drugs’ effects on different parts of the human body before testing them in people.
Testing drugs in human tissue may better reflect the drugs’ effectiveness and toxicities in humans. This process could enable researchers to gather data to accelerate the drug approval process and subsequently make new treatments available sooner to patients.